Lung Transplantation
When lungs fail, both the quality and longevity of life are at risk. A number of disease conditions can cause irreversible organ damage requiring the replacement of the diseased lung (Double/Bilateral Lung Transplant). Children & certain adult with congenital heart defect that have been treated late or are inoperable do end up with irreversible pulmonary hypertension. These individuals will be candidates for a Heart and Bilateral lung transplant as corrective therapy.
Benefits of Lung Transplantation
Lung transplantation has the potential to both lengthen life expectancy and substantially improve quality of life. It is impossible to predict how long you may survive after transplantation. The most critical period for survival is the first year after transplant. This is the period when the risk of post-surgical complications, rejection, and infections is highest. Patients who survive the first year generally survive for five or more years after transplantation. There are even patients alive today who had lung transplantation 10 or more years ago.
Pre-Surgery
A variety of testing is undertaken at the outset to assess the state of your lung and general health.
Lungs
Chest CT to get a 3D X-ray picture of your lungs
PFT to measure lung function
Ventilation-perfusion scan to determine the degree of irreversible damage to the blood and air supply of each lung
Cardiopulmonary exercise testing
DLCO to measure oxygen extracting capacity of lungs
Heart
ECG - This test records the rhythm of the heart
ECHO Doppler -This test uses sound waves to look at heart size and how the heart muscle and valves are working
Cardiac catheterization - It is an inpatient procedure, done to measure the blood pressures in the lung and the heart. It is done with the patient under sedation {administered by an anesthesiologist) and requires a catheter to be placed through a large vein into the heart and dye injected through the catheter while X-ray is taken
Prior to the transplant, your family will meet one of the team’s transplant doctors and transplant nurses who will educate you about lung transplants and answer any questions. We encourage you to ask the transplant team questions any time during the course of your stay. You will also meet our transplant social worker to review psychosocial issues and concerns, especially those that affect normal functioning and family Issues.
The dietician will perform an assessment of the weight, height, body muscle, and fat stores, and will review your dietary history in detail. Your nutritional status is very important in maintaining health during the waiting period, lowering the risk of the surgery, and aiding in the recovery after transplantation. Finally, you will meet one of our psychologists to review cognitive and emotional functioning of you and your family as a whole. The stresses of lung transplantation make this an important and mandatory part of the evaluation.
Once you are accepted into the lung transplant program, you will be placed on the waiting list for organ allocation. During the waiting period, you will:
Be given regular assessment – Including clinical evaluation and lab work/imaging
Undergo regular pulmonary rehabilitation guided by our team of physical therapy experts that will get you in the best possible physical condition for surgery, with exercise and good nutrition
Be required to quit smoking/ alcohol / other drug use
Be put in touch with social and financial coordinators for help with logistical issues
Be counseled along with your family members at regular intervals about what to expect before, during, and after lung transplantation
Be told what to do when it is your time to receive a donor organ
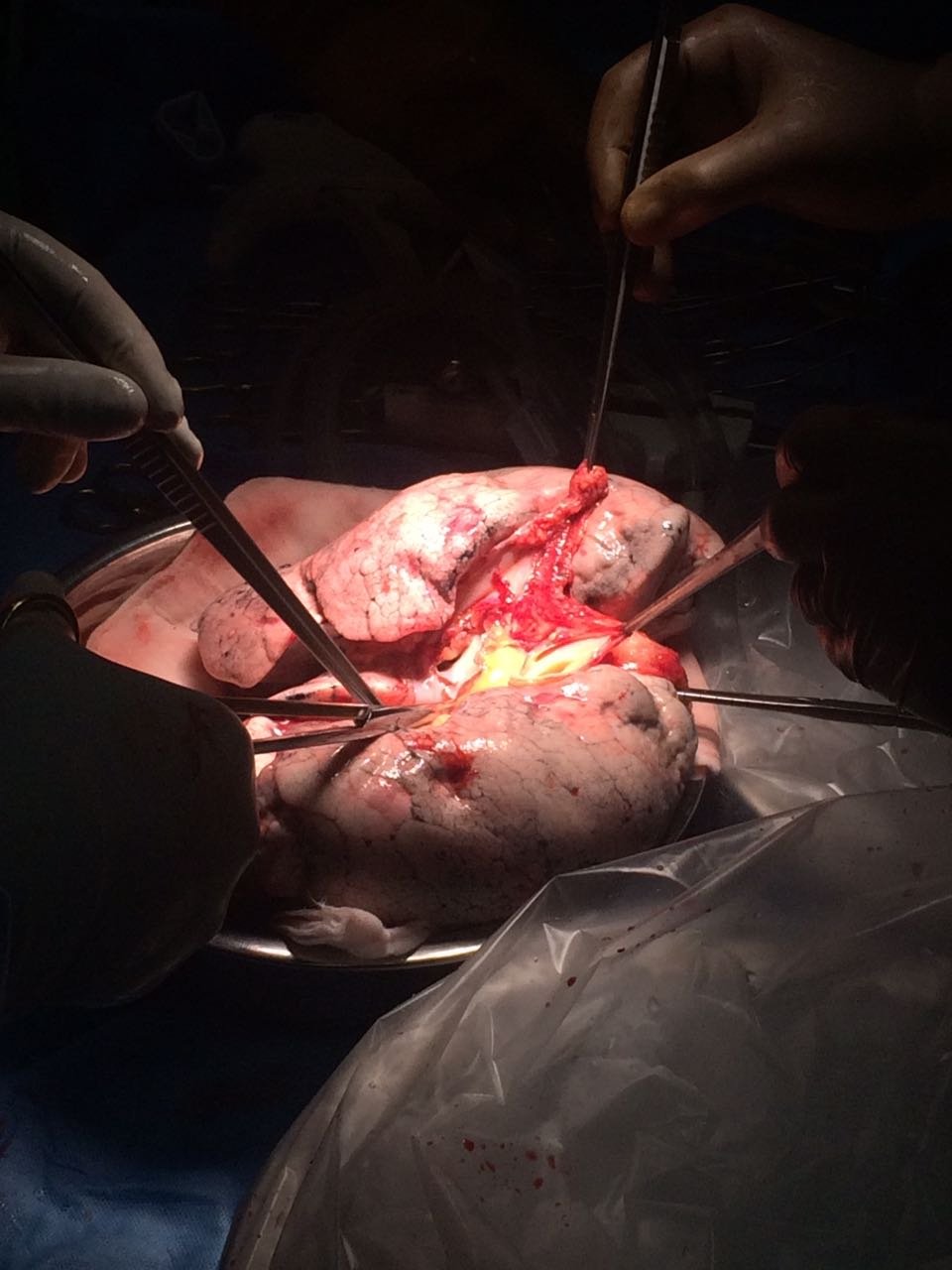
Organ Allocation
When an alert for a potential matching organ for you is received by the hospital through the authorities, you will be immediately alerted to become nil per oral i.e. stop eating /drinking till further notice. The retrieval team travels to the donor hospital to assess the quality of the organ. They perform a series of tests including Bronchoscopy, Trans Esophageal Echo, and Gram Stain among other tests to rule out colonization and airway infections as well as serial blood gas assessments before finally verifying its physical and structural integrity. On confirmed allotment of the organ (based on waitlist status, blood group, size match, and most importantly the quality of the organ) you will be called to the hospital and once again explained in detail about the risk and benefit of lung transplant surgery, its attendant risks. Once your consent is obtained, you are shifted to ICU in preparation for the surgery which involves the collection of blood sample, placement of IV access lines, shaving and clearing of body parts, and shifting to the operating theater.